Introduction
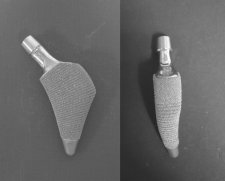
In an effort to reduce stress-shielding and thigh pain as well as to improve survivorship, a new short, metaphyseal-fitting cementless femoral stem (Proxima, DePuy, Leeds, UK) was developed. This new stem is made of titanium alloy and is entirely porous-coated, with sintered titanium beads having a mean pore size of 250 microns, to which a 30 micron thick hydroxyapatite coating is applied, except for the distal tip (Fig. 1). It provides vertical stability by the wedge shape of the stem together with the addition of a lateral flare and preservation of the femoral neck. The preservation of the femoral neck provides greater torsional stability and reduces distal migration of the femoral stem. The absence of any diaphyseal fixation attempts to achieve proximal load transfer so as to reduce stress shielding and thigh pain. It also attempts to preserve the femoral canal and femoral elasticity, and ease revision.
The device in use
Preoperative planning
Pre-operative templating should be carried out to evaluate femoral and acetabular sizing (Fig. 2). However, the philosophy of this implant is different from a conventional stem and size choice is strictly dependent on the bone quality. The femur should be slightly internally rotated for the A/P X-ray. Templating should be preformed both in AP and axial views. A true lateral view should also be obtained to assess the fit of the implant and filling of the femoral neck. The Proxima stem philosophy is not to fill the metaphysis. In the A/P X-ray, the implant should be positioned centrally within the canal allowing a good cancellous margin medially and laterally.
Surgical Approach
Exposure may be achieved using a posterolateral surgical approach to provide optimal visualization of the acetabulum, the femoral neck and the proximal femur (Fig. 3). The “Round the Corner” technique for femoral preparation allows maximum soft tissue preservation and protection of the abductor tendon insertions. The advantages of the "“Round the Corner” technique are even more evident with minimally invasive surgery.
Neck Resection
Neck resection is higher and more horizontal than for conventional THR, extending from the piriformis fossa to the head-neck junction (Fig. 4). Resection may be performed either prior to or after dislocation, depending on the chosen surgical approach. A knife may also be used to release any tissues from around the head and neck. Once the femoral preparation is finished, neck preparation may be completed using the calcar miller with the final broach in place.
Acetabular Preparation
The key points in acetabular reaming are as follows:
- The creation of a hemispherical cavity with uniform bone-implant contact.
- An adequate press-fit for initial stability
- Placement of the prosthesis at the anatomic centre of rotation of the hip joint, whenever technically possible.
- The transverse acetabular ligament provides a useful guide to the orientation and placement of the cup.
A reamer that is 6-8 mm smaller than the anticipated acetabular component should be used initially to deepen the acetabulum to the level determined by preoperative templating. All reamers should be introduced in 40º-45º of abduction and 15º to 20º of anteversion (Fig.5 and 6).
Canal Entry
A dedicated canal finder awl is included in the instrument set. The awl should be placed in the centre of the postero-lateral quadrant of the resected neck to open up the femoral canal (Fig. 7). The tip of the awl is initially directed laterally until the lateral flare is identified and then turned through 180º and advanced down the femoral canal. The proximal metaphyseal cancellous bone may be compressed by moving the canal finder medio-laterally (Fig. 8). The box osteotome is used only when very hard cancellous bone is encountered laterally, but should never invade the greater trochanter or the glutei insertion (Fig. 9).
Broaching Initial Non Anatomic Cavity Preparation
Following definition of the entry point and intra-medullary canal, the cavity initiator (S) broach is used to define the initial femoral envelope. “Round the Corner” is the term used to describe the movement devised to prepare the proximal femur for insertion of the stem. With this technique the surgeon is able to protect the soft tissues, maintain the cancellous bone and provide the best possible load delivery on the lateral flare. The cavity initiator (S) broach is first inserted at an angle of 20º-30º to long axis of the femur (Fig. 10). Once the lateral edge of the broach is below the greater trochanter, the broach is progressively aligned to the axis of the femur. Tilting the broach is achieved by hammering on oblique portion of the strike platform and only a gentle pressure should applied to the handle (Fig. 11). Broaching stops when neutral (or slightly valgus) alignment is achieved (Fig. 12). Excessive force applied to the handle to gain alignment can cause a proximal femoral crack and should be avoided. Removal of the broaches is achieved with the same “Round the Corner” movement.
Alignment Check
The Proxima stem is a conservative implant with no diaphyseal stem extension to facilitate alignment. For this reason an external alignment system, consisting of a long extensible rod which can be quickly attached to the broach handle has been introduced and should be used frequently during broaching, the alignment guide orbits the axis of the femur without pointing at any particular feature of the femur. Instead, when used as intended; the guide helps to align the axis of the broach or the implant with the axis of the femur by verifying that the axes in question are parallel to each other. Accurate alignment is achieved when the axis of the rod is parallel to the femoral axis in two perpendicular planes (Fig. 13). The broach or the implant is correctly seated in neutral alignment when the rod of the alignment guide is parallel to the long axis of the femur in both the sagittal and coronal planes.
Intraoperatively, the surgeon must identify the diaphyseal axis of the femur and use it as a reference. The easiest and most reproducible way is to use proximal and distal femoral landmarks. When parallel in the two planes, if the alignment rod is rotated and superimposed on the medial side of the greater trochanter (proximal femoral landmark) the guide will point at the centre of the knee (distal femoral landmark) and an imaginary line drawn between these two points replicates the diaphyseal axis (Fig. 14). It is also possible to move the alignment guide to a perpendicular position against the broach plane and make sure that the alignment guide points at the medial femoral condyle (Fig. 15). It is then parallel with the long axis of the femur.
Broaching-Sequential Anatomic Preparation
Sequential broaching is carried out with the left or right first anatomic starter (SL, SR) broach. The first of the anatomic broaches enlarges the existing femoral cavity and provides an anatomic profile. This is further enlarged to the required size by subsequent broaches sized.
“Round the Corner” broaching is used to prevent excessive removal of trochanteric bone, and allows the broach to follow the natural geometry of the proximal femur in both the A/P and M/L planes (Fig. 13, 14 and 15). The broach is introduced at an angle of 20º-30º to the long axis of the femur and along the medial curve of the metaphysis. It should be brought into neutral alignment after the lateral edge of the broach is below the level of the greater trochanter (Fig. 16). Care should be taken to preserve or restore femoral neck anteversion and to follow the shape of the proximal femur in three dimensions (Fig. 17). Check that each broach is accurately aligned after seating. All broaching should be carefully performed and any aggressive movements avoided. A dedicated rasp may be used to help facilitate initial broaching if sclerotic bone is encountered anywhere within the region of the broach envelope.
Broaching-Final Anatomic Preparation & Calcar
Sequential “Round the Corner” broach continues from the size 1 anatomic (1L or 1R) broach. The final broach should fit the proximal femur, making sure sufficient good quality cancellous bone is left and rotational stability is achieved. The final implant size will correspond to the final broach used. The alignment of the broaches should be checked at regular intervals and adjusted if necessary. Final seating is achieved by impacting the broach in the axis of the femur. An intra-operative X-ray to check for correct sizing and alignment may be obtained at this stage.
Once the final broach is fully seated and after leg length discrepancy has been checked, a calcar miller may be used to level the neck cut with the level of the porous coating (Fig. 18). A calcar miller with "captured” cutting-teeth is available as part of the instrumentation. As previously advised preservation of the neck may reduce acetabular exposure. In such cases, milling the neck first may significantly help with acetabular preparation and cup positioning.
Trial Reduction
The correct combination of standard or high offset neck trial and modular head are selected to reproduce the patient’s natural biomechanics as determined at pre-operative templating (Fig. 19). To optimize joint function and to increase stability, the largest diameter head possible is usually selected (Fig. 20). A trial reduction is performed and the hip assessed through a full range of movement to identify any instability or impingement.
Final Implantation
The definitive Proxima stem is introduced into the broach envelope with the same “Round the Corner” technique, using the stem inserter/impactor (Fig. 21). The implant must follow the path of the last broach. The final implant should be seated (initially preferably by hand) as far into the broach envelope as possible without undue force. Before final impaction, it is crucial to use the alignment guide to confirm that the stem is in neutral alignment (Fig. 22). Final seating is achieved with impaction in line with the femur.
Impaction with the inserter/impactor is completed when the implant cannot progress any further and the porous coating is level with or just proud of the resected neck. A change in pitch will be noted by the surgeon during impaction when final seating has been achieved. Over impaction of the definitive implant into the canal must be avoided. A further trial reduction must be performed to confirm final position. After trialling is completed, the taper must be irrigated and cleaned to ensure it is free of debris before lightly impacting the selected femoral head (Fig. 23).
Postoperative Rehabilitation
All patients are allowed to stand on the second postoperative day and then progress to full-weight-bearing activity with crutches as tolerated. They are advised to use crutches for 6 weeks and to use a cane thereafter if needed.
Results
114 primary total hip arthroplasties (THAs) have been performed in 100 unselected, consecutive patients less than 50 years old (mean, 43.9 ± 6.11 years; range, 25 to 50 years) and 112 primary THAs were performed in 100 unselected, consecutive patients more than 70 years old (mean, 78.9 ± 12.1 years; range, 70 to 91 years). Only patients with severe osteoporosis were excluded. Osteonecrosis (61%) was the predominant diagnosis of THA in the young patient group and osteoarthritis (52%) was the predominant diagnosis in the elderly patient group.
After a minimum follow-up duration of 5 years, the short, metaphyseal-fitting femoral component has provided stable fixation without diaphyseal fixation in both young and elderly patients (Fig. 24 and 25). No patient has had a revision operation in either group.
References
1. Kim, Y-H, Kim, J-S, Park, J-W and Joo, J-W: Total hip replacement with a short metaphyseal-fitting anatomical cementless femoral component in patients aged 70 years or older. Journal of Bone and Joint Surgery Br 2011; 93: 587-92.
2. Kim, Y-H, Choi, Y-W and Kim, J-S: Comparison of bone mineral density changes around short, metaphyseal-fitting, and conventional cementless anatomical femoral components. J Arthroplasty (In Press).
3. Kim, Y-H, Kim, J-S, Joo, J-W and Park, J-W: A Prospective short-term outcome study of a short metaphyseal fitting total hip arthroplasty. J Arthroplasty (In Press).