Rationale and evidence base for the peripheral vascular use of drug coated balloons (DCBs)
Published date : 27 March 2012
Article date : 27 March 2012
Editorial by Dr Sumaira Macdonald, Consultant Vascular/Interventional Radiologist & Honorary Clinical Senior Lecturer, The Freeman Hospital, Newcastle upon Tyne
Rationale
Paclitaxel, derived from the Pacific yew, demonstrates a “class effect” regarding its impact on restenosis, with favourable results for paclitaxel-coated balloons in four randomised trials of “standard” angioplasty (PTA) versus angioplasty with DCBs and for paclitaxel eluting stents (the Cook Zilver PTX) versus PTA or bare metal stents in the superficial femoral artery. Nevertheless, the efficacy of DCB angioplasty may be dependent on the dose and formulation of the active coating. Whilst sirolimus may have important utility in localised vascular drug delivey, this drug has not yet been trialled.
TRIAL | THUNDER | FEM-PAC | LEVANT 1 | PACIFIER |
DCB | Medrad/Cotavance | Medrad/Cotavance | Lutonix/Moxy | Medtronic/Inpact |
Number of patients | 154 | 87 | 101 | 91 |
Rutherford category | 1-5 | 1-4 | ||
Primary endpoint | 6/12 late lumen loss | 6/12 late lumen loss | 6/12 late lumen loss | 6/12 late lumen loss |
Primary outcomes | 0.4+/- 1.2mm vs. 1.7+/- 1.8mm (p<0.001) | 0.5+/- 1.1 vs. 1.0 +/-1.1mm (p= 0.031) | 0.46mm vs. 1.09mm (p=0.016) | -0.05mm vs. 0.61mm (p=0.003) |
Mean lesion length | 7.5cm | 6 cm | 8.1cm | 7cm |
Diabetics | 50% | 47% | 47% | |
Ca++ (mod/severe) | 46% | 52% | n/a | |
Occlusions | 50% | 13% | 41% | |
Restenosis | 22% 14% ISR* | 27% 7% ISR | 11% | |
12 month patency | 75% | 81% (6 month) | 72% (6 month) |
 The Levant 1 trial (employing the Lutonix Moxy system – the drug eluted is paclitaxel, the excipient is undisclosed) demonstrated superior outcomes in term of six month late lumen loss and follow up is ongoing. The Pacifier randomised trial (employing the Medtronic Inpact system – the drug eluted is paclitaxel, the excipient is urea) again showed superior outcomes with respect to six month late lumen loss and follow up is ongoing.
The Levant 1 trial (employing the Lutonix Moxy system – the drug eluted is paclitaxel, the excipient is undisclosed) demonstrated superior outcomes in term of six month late lumen loss and follow up is ongoing. The Pacifier randomised trial (employing the Medtronic Inpact system – the drug eluted is paclitaxel, the excipient is urea) again showed superior outcomes with respect to six month late lumen loss and follow up is ongoing.  In total there are 8 randomised trials and four registries either enrolling or projected which evaluate the Medtronic InPact DCB. Medrad/Cotavance have five randomized trials in the pipeline, Cook have one on-going randomised trial with the Advance 18PTX balloon (drug paclitaxel, no excipient) and EuroCor have three ongoing randomised trials with the Dior/Freeway balloons (drug paclitaxel, excipient shellac).
In total there are 8 randomised trials and four registries either enrolling or projected which evaluate the Medtronic InPact DCB. Medrad/Cotavance have five randomized trials in the pipeline, Cook have one on-going randomised trial with the Advance 18PTX balloon (drug paclitaxel, no excipient) and EuroCor have three ongoing randomised trials with the Dior/Freeway balloons (drug paclitaxel, excipient shellac). Company | DCB | STATUS | DRUG | CARRIER | TRIALS |
Biotronik | Passeo (18) Lux | Available | Paclitaxel | BTHC* | PEPPER (coronaries) BIOLUX P-I (fem-pop; on-going) |
COOK | Advance 18 PTX | Proposed | Paclitaxel | Undisclosed | SFA trial on-going |
Eurocor | Freeway 14 & 35 | Available | Paclitaxel | Shellac (resin) | Fem-pop trial on-going |
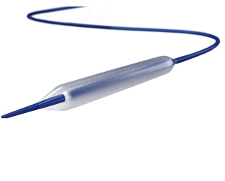
Lutonix | Moxy | Available | Paclitaxel | Undisclosed | 2 coronary trials, LEVANT 1, LEVANT 2 on-going |
Medrad | Cotavance | Available | Paclitaxel | Ultravist 370 (contrast) | FEM-PAC, THUNDER (Copa Cabana, Canal, Euro-Canal, River, Definitive LE on-going) |
Medtronic/Invatec | INPACT Admiral, Pacific & Amphirion | Available | Paclitaxel | Urea | Inpact SFA, Inpact below the knee Leipzig registry; on-going |


