Published date : 27 March 2013
Article date : 27 March 2013
Author: Jim Holland, Consultant Orthopaedic Surgeon, Freeman Hospital, Newcastle upon Tyne, UK; co-authored by Mr Lawrence O’Hara, Consultant Orthopaedic Surgeon, Bournemouth Hospital, UK (No interest declared)
The problem
The
UK National Joint Registry has reported a year on year increase in the numbers of primary hip replacements carried out from 69,000 in 2007 to 84,000 in 2012. Of these, 10% comprise a ‘revision burden’ where failed hip arthroplasties need to be removed and replaced again. Often these cases present with challenging problems for implant removal and reconstruction because of the damage caused by the failing implant material to local muscle and soft tissue. Not surprisingly complications following revision surgery are roughly double those of a primary procedure and outcomes are poorer.
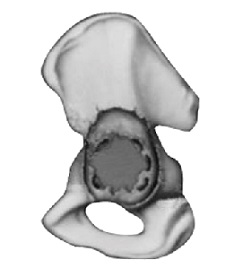
One of the main challenges for revision surgeons is to restore a secure, stable acetabular reconstruction in the presence of a deteriorating quantity and quality of bonestock, often in elderly patients.
A solution
Registry data suggest that on the whole uncemented (bony ingrowth) components are better for revision. These components need to be securely rigidly fixed and allow rapid and reliable bony ingrowth. High strength, high coeffient of friction, iso-elasticity with host bone and biocompatibility are all key properties of tantalum trabecular metal components (Zimmer USA).
What is trabecular metal?
The material:
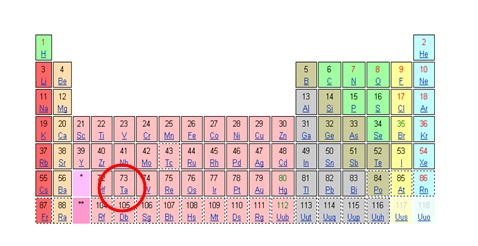
Trabecular metal components are manufactured from tantalum. Tantalum is:
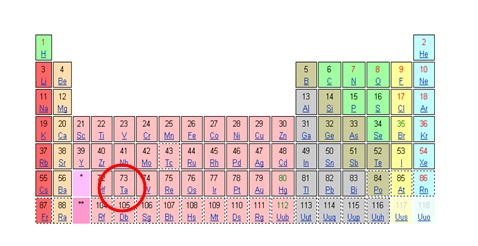
- A pure metallic element, atomic number 73
- A strong, ductile metal similar to titanium
- Highly biocompatible
In 50+ years of clinical use:
- Cranioplasty plates,
- radio opaque markers (RSA),
- pace maker leads, ligation clips etc
Characteristics of ‘trabecular metal’
Trabecular metal comprises 3-D trabecular structures chemically fabricated from Tantalum Metal. This structure has the following characteristics:
- 80% porous for maximal ingrowth
- Elastic modulus similar to bone
- Capable of physiological load-bearing
- High friction and stability with bone
- Osteoconductive porous scaffold
Porosity
The porosity of Trabecular Metal (at 75-80% porous and a pore size of 400-600 µm mimics the structure of cancellous bone and allows maximal bony ingrowth to incorporate the component to the skeleton.
Elastic modulus
Trabecular metal has an elastic modulus or stiffness very similar to and therefore compatible with bone (Bobyn et al 1999).
Strength
Trabecular metal withstands physiological loads and in compression, tension and bending, is comparable to porous metals of higher density and superior to cancellous bone (Zardiackis et al 2001).
Friction
Strut ends of the trabecular structure interdigitate with bone greatly enhancing primary stability which is essential for component fixation and reliable bony ingrowth for a durable construct.
Applications
Trabecular metal has been used in:
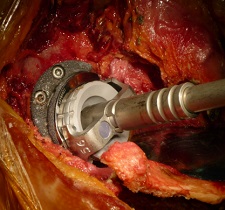
Examples of TMARS (Trabecular Metal Acetabular Reconstruction System) in use:
It is of utmost importance that the correct precribed surgical technique is read, observed and taught before embarking on this surgery. Cadaveric training is regularly available via the
Newcastle Surgical Training Centre, UK.
1. Loose acetabular component with a defect worn into the superior acetabulum (Paprosky IIIA)
Defect filled with augment fixed with 2 screws. Socket impacted anatomically beneath augment and secured with 2 more screws. Bone cement joins the two trabecular metal components to ‘unitise ‘ the construct into one patient-specific modular device.
Bone graft/reamings are used to fill the cavity within the trabecular augment and encourage incorporation.
2. A more severe defect with erosion of the acetabulum superiorly and medially (Paprosky IIIB)
After full debridement, the defect is reconstituted with two augments, face to face, which reconstitute the medial and superior bone loss.
Augments in this case are impacted, not screwed, into place.
The cup is impacted beneath them in an anatomical position, with bone cement again to ‘unitise’ the construct and then screws to secure to host bone of the pelvis.
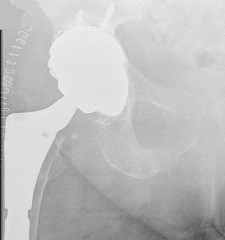
3. Use of ‘buttress’ supero-lateral augmentation device, 2yrs post-op
4. Paprosky IIIC defect, with two medial augments and TM cup, 2 yrs.
Personal experience
2004 – 2012
Total Acetabular cup revisions 273
Trabecular metal cup only required 239 (88%)
Augmentation device required 34 (12%)
(1 failure; inadequate medial support. Solved with cage construct)
Summary
These are reliable and durable components. Their versatility allows bespoke patient-specific acetabular reconstructive options throughout the spectrum of commonly presenting acetabular defects in revision hip surgery.
User comments: Trabecular Metal Reconstruction in Revision Hip Surgery
References